Click here to listen to the blog (3:53).
This year’s Annotated Bibliography of Articles Published in 2022 was just released and includes 113 articles from 33 countries.
Each year, researchers associated with the Prevention Network Action Team (pNAT) of the Canada FASD Research Network search the academic literature for articles related to alcohol use in pregnancy and Fetal Alcohol Spectrum Disorder (FASD) prevention. Articles are reviewed for relevancy, identified by topic and country, and the findings are summarized.
Countries with the highest number of articles published were the US (44 articles), Australia (25 articles), Canada (16 articles), and the UK (13 articles). The findings were organized using a four-part prevention model (below) used by the pNAT to describe the wide range of work that comprises FASD prevention. This year, 48 articles described the prevalence, influences, and factors associated with alcohol use in pregnancy, 12 articles described Level 1 prevention efforts, 32 articles described Level 2 prevention efforts, 13 articles described Level 3 prevention efforts, 13 articles described Level 4 prevention efforts, and 13 articles described stigma, ethical issues, and systemic approaches.
Canada’s 4-part prevention model
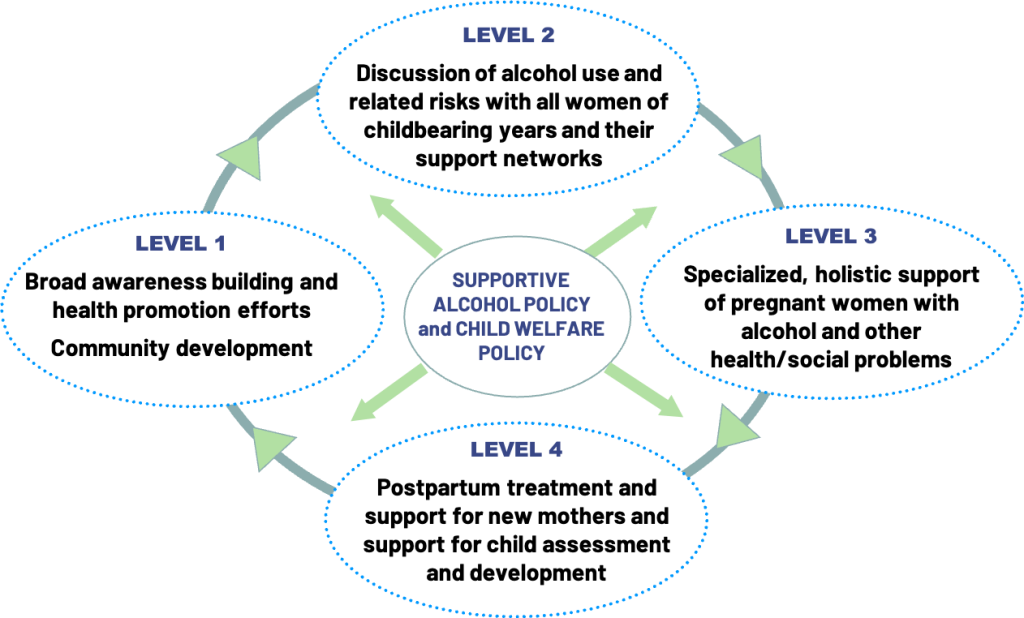
This year we created a category that includes articles describing supportive alcohol and child welfare policy, in which 11 articles were included. An article in this section described the benefits of the Plans of Safe Care initiative (covered in a previous blog), where nearly 90% of participant families were found to avoid out-of-home-placement, illustrating how this program fosters support and creates protective linkages to community-based programs for infants prenatally exposed to substances and their families.
This year, we also saw a shift in how technology was described. In previous years, articles largely spoke to how technology can be used in Level 1 and Level 2 prevention efforts. However, this year, we saw technology also being described in Level 3 and 4 efforts. One study described a virtual peer support program where participants found the virtual space to be a comfortable and safe space where they were able to develop community.
A number of articles considered issues and practices related to screening for alcohol use in the perinatal period. One study captured women’s preferences for specific screening tools (such as the 4P’s Plus), and another explored barriers to disclosure of alcohol use and how health professionals can mitigate these through relational practice.
Consistent with previous years, several studies reported the efficacy of brief interventions. Brief interventions developed by/with Indigenous communities were described, including a mobile health one. And in this year’s bibliography, there was more research on the use, barriers and benefits of brief interventions delivered by a range of providers including physicians, nurses, midwives, pharmacists, and nutritionists.
The annual literature search is intended to update those involved in FASD prevention in Canada, so that their practice and policy work may be informed by current evidence. The members of the pNAT also have the opportunity in monthly web meetings to discuss the implications of the findings for their work. You can access the annotated bibliography here, and view previous annotated bibliographies here.